
Dr. Leah & Mike's Infertility Story
Mar 29, 2022"All I want is to be able to give you a child."
The saddest words I have ever received.
Our infertility journey lasted almost 6 years for a few reasons. It's a long story, so let’s begin?
CHAPTER ONE
May 28th, 2015 - I found out about my husband, Mike's, non-existent sperm in naturopathic medical school while observing his sample under the microscope in our sperm analysis class. As everyone was making their slides and commenting on how amazing their individual samples were (sperm under a microscope are quite cool), how many there were and how fast they were moving, I put my first slide down with Mike’s donated sample. I couldn’t see any, so I kept moving the slide around thinking I must have put it on there wrong. I decided to make another one. And then another one. And then my heart started to sink. I finally saw one sperm in my field of view, it was not moving, just limply floating through the medium and it was all alone.
-
I felt like I was hit with a ton of bricks and my heart broke instantly in that moment. We were studying sperm and infertility in class so I knew what this meant and it wasn’t good.
Mike happened to be picking me up that day and when I got in the truck he asked how his swimmers looked. I had to break the news to him that I couldn’t find any sperm. Best case scenario it was a fluke. Worst case scenario, we may not be able to have kids. It was was one of the worst days of my life.
There was absolutely no evidence he would have an issue with sperm. Let's just say his male parts were very much intact and working well ;) It was a complete shock to both of us.
-
My doctor-mind kicked in, however, and I thought, "You have been using the sauna a lot lately. Maybe that's it. Let's just stop the sauna and recheck. That HAS to be it!"
CHAPTER TWO
It takes 3 months to make sperm. So if you make any change in a male's life, you won't see the effects on their sperm for at least 3 months.
After stopping the sauna and taking all of the right supplements, we re-checked his sample. Still no sperm, at least none that were alive. It was another devastating blow. My theory wasn’t correct. It wasn’t just the sauna.
-
I was still in naturopathic medical school and although we found out about his sperm in my second year, we weren't actively trying. We decided we weren't even considered an "infertile" couple until we had tried for a year.
So we did. I tracked my cycle and we tried a lot. For an entire year.
And my period came like clockwork for 12 months in a row. Now we were considered "infertile" and could seek out infertility care. Yippie for us!

I just knew…
…there had to be a root-cause. As ND's we often find the root cause to things many other doctors can't or don't. There is always an explanation for imbalance, whether it’s physical, emotional, or spiritual; whether you can figure it out or not. Sometimes we don’t have the technology to test or the knowing yet to investigate something unknown, but I believe there is always a reason for imbalance in the body. Finding the root-cause was why I was devoting 8 years of my life to become a naturopathic doctor.
I was a naturopathic medical student full of energy, passion, and determination. And I was determined to figure this one out.
-
So we decided to start seeing whoever we could in the integrative space to figure out what was going on. We thought,
“Maybe it's his gut, let's work on that.”
“Maybe it's his hormones, let's work on that.”
We saw so many doctors, some who said they specialized in sperm health, some in gut health. We went to whoever I felt could help us.
Yet his sperm samples remained unchanged.

CHAPTER THREE
It was time to seek out a conventional fertility specialist.
At this point, a bilateral varicocele was diagnosed. I knew it! I knew there had to be something at the root. I thought, “This must be it.”
As ND’s we are taught to use surgery as a last case scenario, or when its use is the thing that will bring the least amount of harm to the patient, such as an appendectomy. Surgically removing an infected and inflamed appendix is way safer to the patient than trying to cure it with herbs.
I knew that sometimes surgery is the only answer. So we ended up going ahead with the procedure to surgically fix his varicoceles.
-
Sperm take three months to be made, remember…
So after the surgery, we had more waiting to do. After the time was up, we re-tested.
Not only did the bilateral varicocele surgery not work, sperm results were actually worse than before. And now he most likely had scar tissue that may complicate things further.
We were devastated.
At this point, almost two years had passed. I had recently graduated naturopathic medical school and was a doctor myself. No one was helping us, so I decided to take matters into my own hands.
Because my speciality is finding the root-cause for imbalances, I run a lot of labs on patients. You can say I am quite thorough. As a new doctor, I ran a comprehensive lab panel for him to look at more than what any other doctor was looking at.
One shocking marker I found was an elevated homocysteine of 25. Just for context, I am concerned if a patient has a level above 12.
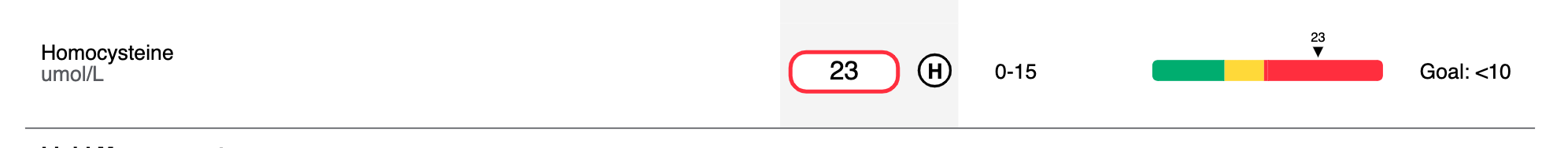
Because of the role homocysteine plays in the body and with my in-depth understanding of biochemistry, I knew that this meant either he was not getting enough B12 and folate or he had a high toxic load. This means that he has so many toxins in his body that his detox pathways can’t keep up. Both of these issues can cause this marker to go up.
CHAPTER FOUR
Because I suspected toxicity…
…I ran a heavy metal and environmental toxicity panel on him. He had high levels of pesticide metabolites, plastic metabolites, phthalates, some elevated lead levels, and one of the highest levels of mercury I had ever seen. Bingo.
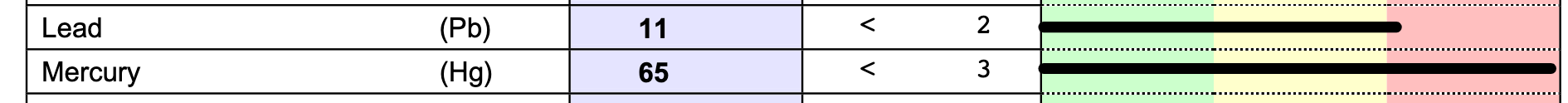
Toxins, including pesticides as well as plastic metabolites and heavy metals, are some of the most pervasive causes of sperm issues. This had to be it.
So much time had already passed, and we had a long road ahead of us chelating the heavy metals out of his body and doing a major detox.
-
For 3-4 months, Mike went into my colleague's clinic and received IV nutrients + chelating agents one - two times a week. He practically lived in our newly purchased at-home sauna so he could sweat out as much as he could.
I had him on a stellar detox protocol, he was taking the best supplements on the market, and eating super clean.
-
After 6 months of this detox to get the toxins and metals out, we had to take another 3 month break from the detox and sauna to see if all of this improved his sperm. The sauna itself, although important for detox, actually affects the sperm. So we had more waiting to do. Again…
We checked again. There was still no sperm, at least none that were alive.
We were heartbroken all over again.
At this point, I didn't know what to think. The fertility specialists said there is always a chance he has sperm in the testicles and that IVF with testicular retrieval and ICSI may be possible.
There was also a chance he would have no sperm there, or it would be highly damaged and unable to create a healthy embryo and baby.
Our options at this point were:
1) We could do testicular mapping to see if there were any sperm in the testicles, but there was a chance it could damage his testicles.
2) We could get a DNA fragmentation test to see how affected his immotile (non-moving) ejaculated sperm really were and if they could be used in ICSI to make an embryo.
3) We could go ahead with IVF with testicular retrieval and ICSI, hold our breath, and pray.
All of it was expensive. Most of it was incredibly invasive. None of it seemed fair.
CHAPTER FIVE
Why was this happening to us?
Why for so many couples did they just have a fun rendezvous under the sheets and 9-10 months later welcome their child into the world? How was it that people who weren’t even trying became pregnant. Why did people who didn’t even want a baby get pregnant every single day?
We wanted to be parents more than anything. I knew Mike especially would be the MOST amazing dad. And he wanted biological children of his own. I wanted the chance to see the love of my life in my children's eyes.
We weren't ready to give up, though.
We decided to do the DNA fragmentation test of the ejaculated sperm because it was more data and it wasn't invasive.

The results didn't look good. Of the very few sperm in his semen sample, not only were they not swimming well (poor motility), they were highly fragmented.
This means most of them didn't have healthy DNA so most likely they wouldn't make healthy embryos that could survive, let alone become healthy children.
Ejaculated sperm were out, even if we went forward with IVF.
-
Our only option…
…was to see if there were any healthy sperm to be extracted from the testicles themselves.
We thought long and hard on what this would mean. We would have to go forward with IVF and they would have to do an invasive surgery to retrieve sperm from inside of his testicles and pray there were some there.
If there were any there, they would need to be injected physically into my retrieved eggs in the hopes of making an embryo, aka ICSI. This was after weeks of me taking medications to manipulate my hormones to make more eggs, something was I literally helping people avoid every day in my natural fertility practice.
But this was our only chance at becoming biological parents together.
-
This was really hard for both of us to accept. We had to mourn the loss of the idea of having children naturally, or possibly biological together.
I am a naturopathic doctor, I try my best to avoid invasive or conventional medicine unless absolutely necessary. I trust the innate wisdom in the body.
I help women become pregnant naturally all of the time and I help them get off medications, such as birth control. I didn't want to take synthetic hormones to become pregnant when I knew way too well what they can do to the body. I knew way too well what hormones like birth control did to me. I didn’t want to induce another round of depression as I had experienced years prior when I was taking the pill.

It all felt so unfair.
This rocked my world and it took me a long time to process it all and come to peace with the idea of IVF. I spent many years and many hours seeing therapists and healers, processing the infertility and my thoughts about IVF.
And after knowing we could spend over $30,000 + and it still may not work, we decided to move forward anyway and pray that it did.
CHAPTER SIX
We finally decided we were ready to pursue IVF since it was our only chance of becoming biological parents.
Keep in mind, I did my very best to stay out of conventional doctor’s offices. Usually their go-to tools were medications and surgery, two things I usually avoided as much as I could, and they often didn’t take the time to find the root-cause of issues. I usually chose more holistically-minded doctors and dentists.
Being a holistic and functionally-trained doctor, I was also on the receiving end of patients who had ‘not so pleasant’ experiences at the doctor, often being rushed and not being listened to. Patients would share with me that often doctors they saw didn’t seem to care what was REALLY going on. That was literally why people came to see me.
But I digress…
-
We received a referral from our male infertility doctor and started the process with clinic #1.
It all felt so surreal…
…checking in and telling them we were there for our IVF evaluation. I never imagined this would be us.
Because IVF (and fertility / infertility in general) is so focused on the woman, I had to have an ultrasound during our first visit to evaluate me.
I never thought I would have any issues because as far as fertility went, I always thought I was normal. This entire time we were so focused on Mike and his sperm so the focus was never really on me. I had done plenty of my own lab work and ultrasounds to make sure my hormones were normal. Besides low testosterone, higher estrogen, and slightly elevated prolactin, I seemed normal. I ovulated normally and had regular cycles, so I didn’t think I would have any issues.
During the first ultrasound, the doctor told me I had a lot of follicles on my ovaries. I had been told that before in past ultrasounds, but I was told it meant I was really fertile. She told me I had a variant of PCOS (Polycystic Ovarian Syndrome). I knew I didn’t have actual PCOS because I had low testosterone and regular cycles, two things that are often not a part of PCOS. I now know I have what is called PCO, polycystic ovaries, but not PCOS, the syndrome.
Regardless, I learned that day that this fact would make IVF much more complicated since I was at risk of hyper-stimulation, which is what sends most women going through IVF to the hospital. It turns out if you are younger and have a lot of eggs, aka more fertile, you actually make IVF more complicated and risky because of the medications they use to trigger egg maturation during the egg retrieval process. Lovely.
I also discovered that day that I had a uterine polyp that would need to be removed through surgery prior to implantation. That was new.
My heart started to sink and she began to really annoy me…
…as she continued to go through the list, placing the blame on me for our infertility, despite the fact that we KNEW my husband had no sperm.
She mentioned I should do a test to look at my fallopian tubes, a Hysterosalpingography, or HSG. I am all about doing tests, but that one involved contrast media and an x-ray and I was already so sad that I had to take medications to become pregnant, subjecting my uterus and ovaries to that prior to IVF felt so unnecessary and potentially harmful to all of my eggs. We knew we were going to do IVF with testicular retrieval so why did I need that?
I shared that we were fairly certain we weren't getting pregnant due to the complete lack of viable sperm and asked what value would it bring us to do the test? She said if there was an issue, they would simply remove the fallopian tubes at that time.
She said it so casually, like it was as simple as afternoon tea.
I knew in that moment what it was like to be a patient of mine having their experiences in the conventional medical model. As soon as she left the room I couldn't hold it back any longer, I just lost it. I had been so strong up until this point, rarely crying in front of Mike because I didn't want him to feel bad, but the idea of me going through IVF, being at a higher risk, having to go through another surgery, and the doctor feeling like she could just casually remove my fallopian tubes sent me over the edge.
When the financial lady came in the room I pulled myself together as she went over the $30,000 + commitment it would be.
It was not the best day of my life.
CHAPTER SEVEN
After feeling uncomfortable at our first IVF clinic, I decided to ask around for other referrals.
I interviewed another doctor who supposedly specialized in male-factor IVF and PCOS. She seemed ok.
Another recommendation led us to clinic #2.
This experience was a little better than the first. The doctor seemed to know more and was more open to explaining things, which I appreciated. I felt a little more comfortable, so we decided to switch.
At this point, spiritual guidance started playing a larger and larger role in our process. Through a medium/intuitive I LOVE, I was able to connect with our baby souls and learn that this process of infertility and needing to go through IVF was all in our life plan; it was supposed to be this way. She also said when she tuned into Mike, she felt the sperm were there but they were getting trapped in a maze, they were stuck. We didn’t know what to make of it, but it gave us hope.
Mike also had a crazy dream that he felt was more of a spiritual message than a typical dream. During the dream the angel of death showed him something that he intuitively thought meant there was life inside his testicles, even though it looked like death from the outside. We didn’t know how or if that could be true, but we were hopeful.
We finally decided on a doctor at this second clinic. It had been 5 years, we were ready to begin. On my next period I was supposed to call so I could start my bloodwork, ultrasounds, and medications.
-
2 weeks later the COVID lockdown began.
All IVF was canceled until further notice.
All that kept going through my mind was, "Are we just not meant to be parents? Why is this happening! It shouldn't be this hard."
We were thrown into yet another situation that was out of our control where we had to surrender. We were starting to get good at accepting the uncontrollable.
This is why they call us #infertilitywarriors
-
So the COVID lockdown continued.
Once they started to open up medical clinics a few months later, our clinic was taking only high risk cases, in particular women with cancer who needed to retrieve their eggs prior to chemo. Our clinic happened to specialize in that so they was not going to be available for us. Lucky us.
We were not a high priority, understandably so, but it wasn't looking good. Months went by and I finally decided to look elsewhere.
A colleague of mine recommended Dr. Chang at Hanabusa IVF, one of the pioneers in mini IVF, a lower dosed and more natural approach to IVF. This sounded right up by alley.
Ironically, I had actually come across him months prior when I found out about my PCO, and had considered seeing him, but I went with the recommendations for the other two clinics from friends instead. My soul was pointing me along the right path all along, I just wasn’t listening closely enough. But eventually we came full circle in September 2020 when I met with him.
-
Right away I loved his energy…
…he respected my field, he cared so much, and his approach was more integrative. I was sold. I knew this was right, I actually trusted him, which was so important for me in this process. With all of the spiritual support I was receiving, I was starting to learn the feelings of when I was on the right path. This was it.

CHAPTER EIGHT
In preparation for IVF we decided to do genetic carrier screening, to make sure we didn’t share any variants of genetics that could lead to diseases in our future babies.
I decided to send mine off first because if I didn’t have any recessive gene mutations, Mike wouldn’t need to do it since the concern is only if we both carried a genetic mutation.
I received my carrier screening test back and I had one mutation. Lovely. It would only be an issue if Mike also carried that gene mutation. We needed to get him tested after all.
-
I ordered the genetic carrier testing…
…because I am a doctor and I could. That means I received the reports with the detailed explanation that most doctors leave out of their visits with you.
When we got Mike’s back, he was negative for my genetic mutation, but he was positive for a few others including the CFTR-associated disorders variant.
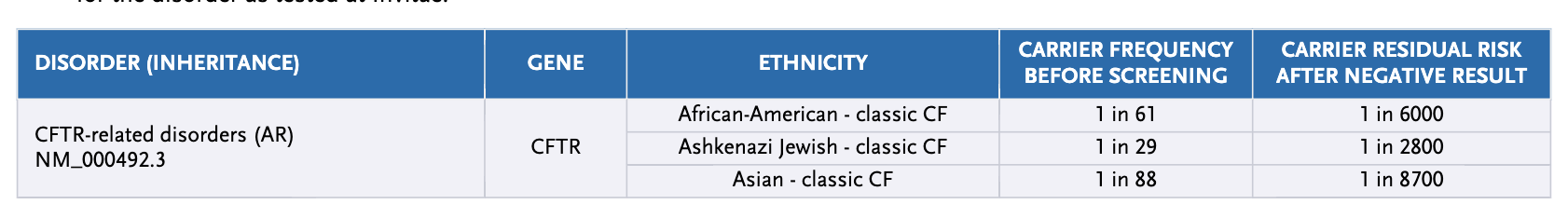
I was taught in school that if egg and sperm both pass a CFTR gene mutation to their child, they can develop cystic fibrosis, a disease that mostly affects the lungs. The report, however, mentioned that his type of variant was associated with a condition called: congenital absence of the vas deferens.
The minute I read those words my whole world stopped.
What! How did we not know this? How did our fertility doctors not mention this condition?
I frantically started reading about it. Men with this variant can have issues with their vas deferens, the tube that allows sperm to travel from the testicles to the outside world. Essentially, Mike most likely has had an inborn vasectomy, a procedure where one surgically cuts the vas deferens as a form of birth control. The thing is his may have been there since birth. This means sperm have a hard time getting out, or can’t get out at all.
I couldn’t believe it. This diagnosis would also confirm Mike’s dream and the spiritual guidance telling us that there is life inside, it’s just getting stuck. I had so much peace going into IVF now because I knew this REALLY was the only way for us to become biological parents together.
I had hope again.
There was still a chance he wasn't making sperm at all, but again, we prayed he was.
I wondered, “Why hadn’t this come up sooner? Why hadn’t someone mentioned this as a possibility? Why hadn’t I found it. Would it have changed our journey?”
I believe we didn't find out about it prior for a reason. Infertility has taught us so much, lessons we were meant to learn.
With that knowledge…
…we decided to move forward with a mini-IVF cycle in October 2020.
I was shocked when I went to the pharmacy to get my "lower dose" protocol and it was $5,000. I understand why infertility treatment is not accessible to everyone. We don’t have regular insurance since we are both self-employed, however most insurance doesn’t cover IVF anyway.
We had been saving for years just in case this was the route we had to take. We delayed buying a house for years so we would have enough cash saved up for IVF. So although it was a massive sticker shock, we kept going.
-
I started alternating an injectable hormone with an oral one going in every few days for bloodwork and an ultrasound. They monitored my follicles closely so I wouldn't hyper-stimulate but would have enough for transfer. This was the key with “mini-IVF.”
Dr. Chang's approach with eggs is lower quantity, higher quality.
That made sense to me. Nutrient resources spread among 15 is better than 30.
After two weeks on hormones, my follicles were ready for transfer! We had about 15 follicles that could become eggs and I hadn't hyper-stimulated! Yay!

I decided to not use general anesthesia during egg retrieval, which means I could feel it all. It seemed like a good idea at the time, Dr. Chang encouraged it, and assured me I could handle it. It was one less dose of general anesthesia I would have to take. I am grateful I was awake for the procedure, but it was quite painful and more shocking than I anticipated.
In the end, we retrieved 14 eggs, and I got it on video.
The biggest question mark was Mike's sperm. One day before I went in for my procedure, Mike went in for testicular surgery. They removed testicular tissue to try and find sperm to match with my retrieved eggs. We had no idea what would be there, so there was a chance this was all for nothing, but we were praying it would work out.
CHAPTER NINE
When I came out of my procedure room after the egg retrieval, I was a little in shock from the pain of having my ovaries poked with a long needle 15 times. It was emotional because it was a literal painful reminder of how this wasn’t how I imagined becoming a mom.
I immediately asked to speak to the embryologist because they had been hard at work all day looking for sperm and I wanted the update. This all depended on the sperm.
She shared with me that unfortunately at that point, they hadn't found any sperm in the tissue sample yet that they could use to make an embryo. They said they were going to keep looking and would let us know if they found any.
It felt like I was punched in the face and the gut at the same time. I was absolutely devastated.
I lost it.
Like really lost it. I have never cried so hard in my life.
Because of COVID Mike wasn’t allowed to be with me after my procedure. So I laid on the operating table in the cold and empty room wearing my surgical gown, hair net, and mask, shivering from the shock of my procedure and the news I received that we still may not be parents.
After 6 years, dozens of appointments, thousands of dollars, multiple surgeries, medications that may impact my hormones for life, and half a decade of heartache, we still may not be parents.
This time I wept. I couldn’t stop crying. The nurses didn’t know what to do so they brought me water and let me cry alone.
I was absolutely heartbroken.
-
Mike came and picked me up since I couldn’t drive after that and as we went to the counter to pay another $10,000 for this little procedure, they told us they weren’t going to charge us yet. The energy in the clinic was, “There may not be any embryos, this poor couple, we can’t take their money right now.”
They sent us home and told us they would update us via email over the next few days on results. The fact that they didn’t take our money that day left me feeling horrible. All of my worst fears were potentially coming true.
I cried all the way home.
-
Mike had just had surgery the day prior so he was recovering from that and I was really sore from my egg retrieval procedure and the bloat from the medications. So we both just sat on our couch praying, but also crying, because it was now in Spirit / God’s hands.
We waited impatiently for the single email..
…that would reveal if we were going to have a family together or not.
CHAPTER TEN
I remember exactly where I was when I received the first email update. Sitting on our gray couch in our little 900 square foot duplex two blocks from the Pacific Ocean in Leucadia, California. I was afraid to open it.
I was afraid it would say they didn’t find any sperm.
The report showed:
-
14 eggs collected
-
6 embryos fertilized
They would send us an update over the next few days on if the embryos were progressing past fertilization to become viable embryos.
-
There are so many obstacles in IVF. For many people it can be a struggle at any one or all of them. Getting eggs can be a challenge, we were good there, thanks to my age, health, and the mini-IVF protocol.
Getting sperm was our current challenge.
But we had 6 eggs that fertilized! That meant they found at least 6 sperm. Keep in mind one ejaculate should have 20-30 million sperm, just for context.
The relief we felt was palpable. However, we weren’t out of the woods yet. For anyone who has been through IVF, they know this is just the beginning.
What we didn't know…
…was if the sperm were healthy enough to make healthy embryos. Time would tell us as they either progressed to day 6 blastocysts or not.
-
The way IVF works is they retrieve eggs from a woman after giving her extra medications and hormones to make more of her monthly follicles turn into eggs. Then they use sperm from the man, usually just what is found in an ejaculated sample. In traditional IVF, they put the sperm sample and egg in a petri dish and the sperm naturally find the egg and implant it: the moment of conception. In ICSI, what we did, they manually insert one sperm into the egg to induce conception. Then, they see if that egg and sperm resulted in a fertilized egg. Then, if it did, the cells will start to divide and over the next 5-6 days it will progress to the end result, a day 6 blastocyst. This is the stage when the embryo will be transferred to the mother in a fresh transfer, or frozen to be used in a future transfer in the hopes of it becoming a baby. This same process happens naturally 6 days after conception when you have unprotected sex around ovulation.
The difference between natural conception and IVF is that fertilization and blastocyst growth happens outside of the woman’s body. And every day from fertilization to day 6 blastocyst has high risk of losing embryos.
In the IVF world, it’s often a 50% game.
Meaning however many eggs you retrieve, you fertilize 50%. 50% make it to day 3, 50% of those make it to day 6. 50% of those are normal and 50% of those may or may not implant, depending on other factors.
So when you start with 6, those numbers don't look very good. We were hopeful, but we also started to prepare ourselves mentally for potentially having to do it all again, including Mike's invasive testicular surgery.
We finally received our email that 5 of our 6 fertilized embryos made it to day 6!
This was phenomenal news! Even better than the average, meaning of the sperm they collected, they were really healthy and strong.
I had never felt so much relief and joy in my life.
I also knew that if we had learned about the CF mutation earlier in our journey, we wouldn’t have checked for heavy metals and toxic chemicals and got rid of them. Their presence probably would have greatly impacted the quality of the sperm at the testicular level. We wouldn’t have explored EMF protection in our home and on our technologies that most likely contributed to the DNA integrity as well. It became clear that there weren’t many sperm and they were trapped, but the ones there were mighty!
Now we had to send the embryos off for PGT testing to make sure they were normal chromosomally, ruling out Down Syndrome, Trisomy 21, and other chromosomal issues. This wasn’t necessary given my age, but given Mike’s sperm situation, we wanted to error on the side of caution.
SO…..
The anxious waiting game continued.
The theme of our fertility lives.
-
The day the email came in we were holding our breath as we opened it. Were we going to have healthy embryos? Were we going to have to do this all over again?
Of the 5 embryos, 4 were healthy, 2 boys and 2 girls. I couldn’t believe it. It literally felt like a miracle. I cried, again. This time the tears were happy.
CHAPTER ELEVEN
We now had four healthy embryos on ice. Our next step was a polyp removal surgery for me. Joy.
I do a lot of work with the microbiome and I know how important it is prior to and during pregnancy. Antibiotics unfortunately often disrupt and negatively impact the important microbiomes in our gut and vagina.
The fact that I had to take prophylactic antibiotics for the retrieval and polyp surgery was a hard pill to swallow ;). I took the one for the retrieval because after being awake while they inserted a needle 15 times into my ovary, I didn’t want to risk an infection and losing my ovary for good. I decided against the one for my polyp removal and I did a lot of work replenishing with probiotics and fiber-rich foods.
The surgery went well and my doctor mentioned our chance of a healthy first time transfer was probably higher because they scraped out my uterus. I guess I was grateful for that.
We were aiming for a natural transfer…
…which meant we would implant the embryo 6 days after my normal ovulation. This would mimic what would happen naturally in normal conception. This depended on my hormones being balanced and cooperating to have a normal ovulation cycle.
Before and after my egg retrieval I had run labs on myself to see what was happening to my hormones. They were quite imbalanced after that process, even on the lower doses of hormones and medications, so that worried me. I knew I needed to wait three months between retrieval and transfer because the body usually takes at least 3 months to rebalance hormones. I had a theory that women who did transfers soon after retrievals had higher rates of failed transfers because of that fact.
I used a ton of nutrients and herbs to help rebalance my body and I felt intuitively January was the month to do it.
-
I tracked my cycle, as I always do. I was also monitored closely through bloodwork and ultrasound at my clinic. Once I naturally ovulated, I was set to go into the clinic 6 days later.
One of our embryos was implanted using a little tube inserted through my cervix. I was awake for it and got to see the whole thing on ultrasound. I was told to go home and rest.
From that moment on, it was up to nature, my body’s ability to hold a baby, and what was meant to be.
Since I implanted naturally, one week after this process would be my "missed period" where we would simply check to see if it worked and I was pregnant!
So the waiting continued, this time waiting to taking a pregnancy test! I tried to remain positive as I knew failed transfers were very common in IVF.
But I trusted my body, I knew I was healthy, and it felt like it was meant to happen. I didn’t let myself think negative thoughts or dwell on what could go wrong.
I simply kept giving gratitude for the healthy baby and telling her she was safe and it was ok for her to make a home in my womb.
The day we checked our HcG via blood at our clinic, I couldn’t wait until the afternoon for the results so we decided to take an actual pregnancy test. This was against the advice of our IVF doctor because in those early days, at-home tests can be negative despite still being pregnant.
I was very used to negative pregnancy tests…
…so if it was, I would be fine. I knew the blood test was more accurate.
So we decided to do did it!
In 6 years I had never seen the second line on a pregnancy test.
Seeing that second line was one of the happiest moments of our lives!
CLOSING - CHAPTER TWELVE
Our journey has been unique, trying, discouraging, and hopeful. It has brought up so much of our shadows and has shed light on so many wonderful things.
So many lessons have been learned, both personally and professionally. Mike and I are closer than ever and more grateful for our baby than we could ever imagine.
I never dreamed that my motherhood journey would be like this, but now I can't imagine it any other way.
Pregnancy and birth became our next great adventure. Stay tuned for that story, coming soon.
Thank you for following our journey. I hope you are as inspired as we are.
Dr. Leah


